The majority of the approximately 6 million patients in Germany who suffer from type 2 diabetes are overweight. The effect of insulin is limited in them. For a long time, the cause of this insulin resistance was primarily sought in metabolically active organs. Scientists from Max Planck Institute for Heart and Lung Research in Bad Nauheim and Goethe University Frankfurt have now been able to show that the effects of insulin on the inner cell layer of blood vessels, the endothelium, are of great importance for insulin resistance in fatty tissue and muscles. The key molecule here is the hormone adrenomedullin. With this study, the researchers hope to have found the basis for a new therapeutic principle for type 2 diabetes. The aim is now to develop substances that specifically target the blood vessels.

More than 400 million people worldwide suffer from type 2 diabetes, around 6 million of them in Germany. In nine out of ten patients, severe overweight, known as obesity, leads to diabetes. Type 2 diabetes is characterized by the fact that body cells no longer absorb enough glucose. As a result, the glucose level in the blood rises. Insulin loses its effect, at least in part, and this is referred to as insulin resistance.
In order to clarify the cause of insulin resistance in obese patients, research has so far focused primarily on metabolic organs such as the liver, adipose tissue and skeletal muscles. Receptors for insulin are found in the cells of these organs. So far, however, no therapeutic approaches have been developed to eliminate insulin resistance.
Stefan Offermanns, Director of the “Pharmacology” Department at the Max Planck Institute for Heart and Lung Research in Bad Nauheim and Professor at Goethe University in Frankfurt, and his team have now investigated the role of the innermost cell layer in blood vessels, the so-called endothelium, in the development of type 2 diabetes in connection with obesity.
Although it has long been known that receptors for insulin are also present on endothelial cells, their importance in the development of diabetes has been underestimated until now. “When insulin docks to its receptor on the endothelium and activates it, this leads to dilation of the blood vessels and improved permeability of the vessel wall for insulin. As a result, glucose and insulin can better pass from the blood into metabolically active organs such as the liver and muscles,” explains Haaglim Cho, first author of the study. This has been known for some time.
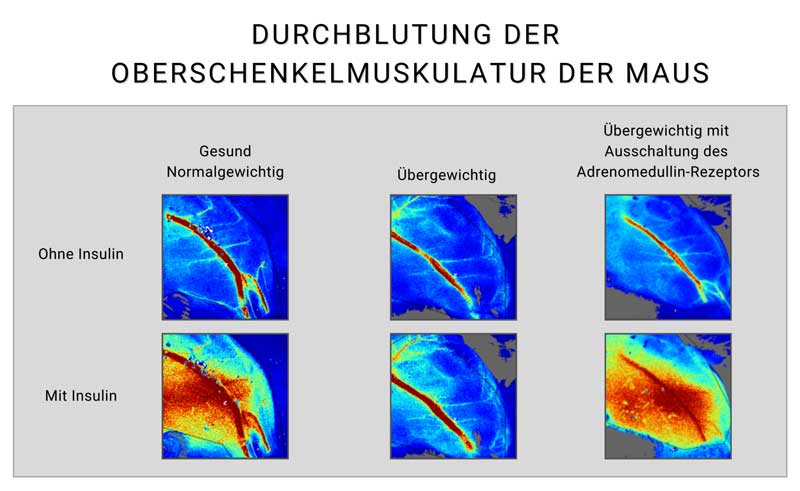
The study carried out by the Bad Nauheim researchers on mice has shown for the first time that this mechanism can be disrupted in the case of severe obesity. “In mice that became obese as a result of a particularly high-calorie diet, insulin resistance developed after some time,” says Cho. “We were able to identify a reduced activity of the insulin receptors of the endothelium as the cause of this.” The results suggest that insulin resistance in the vascular endothelium leads to a reduced insulin effect in the entire organism, as the two mechanisms mentioned above, via which insulin is transported from the blood to the metabolically active organs, are then impaired.
But what is the cause of the development of insulin resistance on the endothelium? Further experiments led the scientists to the hormone adrenomedullin. It is released into the blood in overweight people, particularly from fat cells. “In overweight mice, we found an effect comparable to that in human patients, namely that the adrenomedullin level in the blood is significantly increased. Another protein, complement factor H, is also elevated in the blood of both mice and humans with obesity. Our study showed that both factors reinforce each other in their effect on the insulin receptor,” explains Cho.
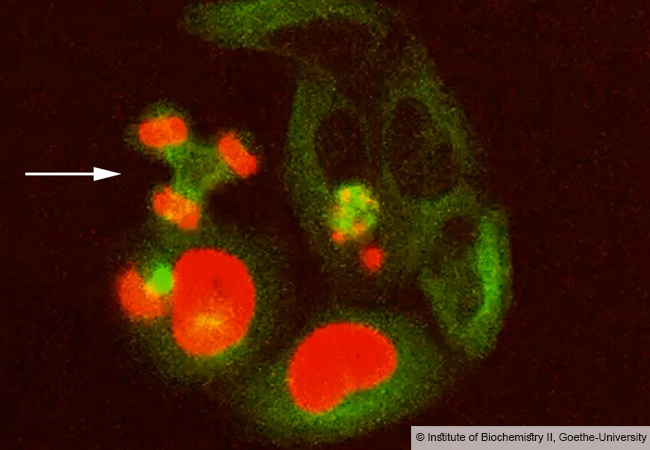
The effect of increased concentrations of adrenomedullin and complement factor H in the blood on the insulin effect was shown in further studies on mice: both factors synergistically activate the receptor for adrenomedullin on the endothelium, thus increasing their effect. The activated adrenomedullin receptor in turn inhibits the insulin receptor particularly strongly. This reduces the insulin effect. “We were able to confirm this finding in healthy, normal-weight mice to which we administered adrenomedullin. This also resulted in insulin resistance,” says Cho. Conversely, mice in which the production of adrenomedullin or the activation of the endothelial adrenomedullin receptor was temporarily prevented by genetic engineering showed a normal insulin metabolism, even when they were overweight.
Stefan Offermanns categorizes the study results: “Our data show the insulin effects in blood vessels and how important the effect of insulin on blood vessels is for the systemic insulin effects.” Above all, the study reveals a mechanism according to which the systemic insulin resistance of type 2 diabetes triggered by obesity is essentially based on insulin resistance in the vascular system. Offermann explains: “We hope that the improved understanding of type 2 diabetes caused by obesity is a first step towards the development of new substances that can be used to treat type 2 diabetes.”
Publication: Haaglim Cho, Chien-Cheng Lai, Rémy Bonnavion, Mohamad Wessam Alnouri, ShengPeng Wang, Kenneth Anthony Roquid, Haruya Kawase, Diana Campos, Min Chen, Lee S. Weinstein, Alfredo Martínez, Mario Looso, Miloslav Sanda, Stefan Offermanns: Endothelial insulin resistance induced by adrenomedullin mediates obesity-associated diabetes. Science (2025) http://science.org/doi/10.1126/science.adr4731