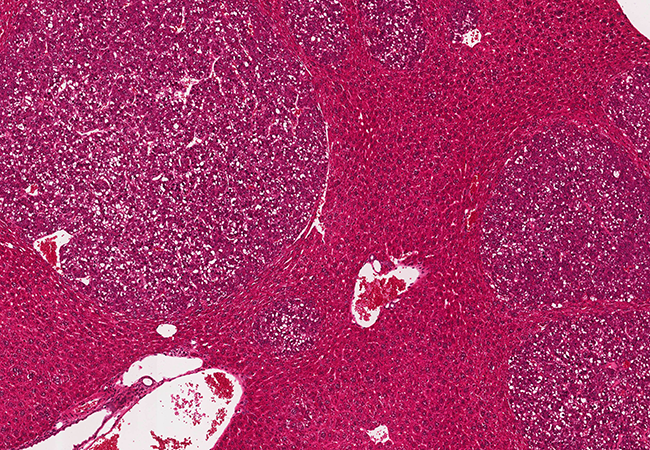
Iron-dependent cell death (ferroptosis) is a type of programmed cell death by means of which the body kills off diseased, defective or superfluous cells. This process can be used to make immunotherapies against liver cancer more effective. Researchers at Georg-Speyer-Haus, University Hospital Frankfurt and Goethe University Frankfurt have now been able to show this in mice with liver cancer. The combination therapy was also effective against colon cancer metastases that had settled in the liver.
Ten years ago, a new type of programmed cell death was discovered: iron-dependent cell death or, to use the scientific term, ferroptosis. Unlike apoptosis, a long-known type of programmed cell death, in ferroptosis the cell absorbs larger amounts of iron. The iron is metabolised in the cell and eventually leads to the destruction of the cell membranes. Such types of cell death are among the body’s important control mechanisms, for example in development processes and the elimination of defective or degenerate cells.
For some years now, immunotherapies have established themselves as a treatment option in the battle against cancer. Here, the body’s own defence system is stimulated so that it acts against cancer cells. A number of these immunotherapies successfully target key points in the immune system, known as checkpoints, where the immune system is subdued.
Immune checkpoints are a kind of “off switch” on the surface of T cells (cancer-fighting immune cells), with which their activity can be down-regulated. This “off switch” is operated by certain “key” proteins. Many tumours form such “key” proteins to protect themselves against attacks by T cells. That is why blocking the “off switch” by means of drugs, i.e. immune checkpoint inhibitors, are now part of the standard treatment in some types of cancer. Unfortunately, in other types of cancer, such as liver cancer, the response to the immune checkpoint blockade is low.
Researchers at Georg-Speyer-Haus, together with University Hospital Frankfurt and Goethe University Frankfurt, have now observed in mice with colorectal cancer that a substance which triggers ferroptosis leads to the activation of certain immune cells (T cells). Such T cells can systematically kill off cancer cells.
The problem was that two independent mechanisms immediately put a halt again to T cell activity: firstly, the cancer cells formed a “key” protein to operate the “off switch” of the T cells (the immune checkpoint receptor PD-L1). Secondly, other cells of the immune system, known as myeloid suppressor cells, came onto the scene, whose task is equally to subdue the body’s immune response.
However, when the researchers gave the diseased mice a triple combination of a ferroptosis activator, an immune checkpoint inhibitor and a substance that prevents the attraction of myeloid suppressor cells, this significantly reduced the liver tumours’ growth.
In further tests on mice, the scientists established that the combination therapy was also able to reduce the number of liver metastases originating from a metastasising colorectal tumour. The colorectal tumour itself, however, did not respond to the combination therapy.
Professor Fabian Finkelmeier, one of the two first authors of the study, says: “The combination therapy is apparently dependent on the liver’s microenvironment and not on the primary tumour. This indicates that our combination therapy could be effective against liver metastases from any type of cancer.”
Dr Claire Conche, the second first author, explains: “With this new combination therapy, we attack the immune system from three sides. First, we make the cancer-fighting T cells reactive towards the tumour cells. Then we remove the obstacles facing the cancer-fighting T cells: the suppression cells and shielding by PD-L1.”
Professor Florian Greten, director of Georg-Speyer-Haus and spokesperson for the LOEWE Centre “Frankfurt Cancer Institute”, says: “The study underlines the pivotal role of the tumour microenvironment in cancer therapy. We have concentrated here on the immune compartment of the tumour microenvironment and how to modulate the immune system in the direction of a strong anti-tumour response. Our data in preclinical models are an encouraging basis for improving immunotherapy options for patients with hepatocellular carcinoma and liver metastases.”
Publication: Claire Conche, Fabian Finkelmeier, Marina Pešić, Adele M Nicolas, Tim W. Böttger, Kilian B. Kennel, Dominic Denk, Fatih Ceteci, Kathleen Mohs, Esther Engel, Özge Canli, Yasamin Dabiri, Kai-Henrik Peiffer, Stefan Zeuzem, Gabriela Salinas, Thomas Longerich, Huan Yang, Florian R. Greten: Combining ferroptosis induction with MDSC blockade renders primary tumours and metastases in liver sensitive to immune checkpoint blockade. Gut (2022) http://dx.doi.org/10.1136/gutjnl-2022-327909