A study by Goethe University Frankfurt points to the possibility that thalidomide derivatives are potentially suitable for treating cancer. Thalidomide was marketed in the 1950s as a sleeping pill. It later gained sad notoriety for causing severe fetal abnormalities in the early stages of pregnancy. It is meanwhile known that the molecule marks proteins in the cell for degradation. For the current study, the researchers produced thalidomide derivatives. They were able to show that these influence the degradation of proteins responsible for the survival of cancer cells.
Hardly any other molecule has a more turbulent past than thalidomide. It was the central ingredient in a drug approved in many countries in the 1950s as a sedative and sleeping pill. However, it soon became apparent that pregnant women who had taken thalidomide often gave birth to children with severe deformities.
For the past few decades, however, medicine has nevertheless pinned great hopes on it again. Studies have shown, among other things, that it inhibits the growth of blood vessels and is therefore potentially suitable for cutting off tumors from their nutrient supply. It then also proved very effective in the treatment of multiple myeloma, malignant tumors in the bone marrow.
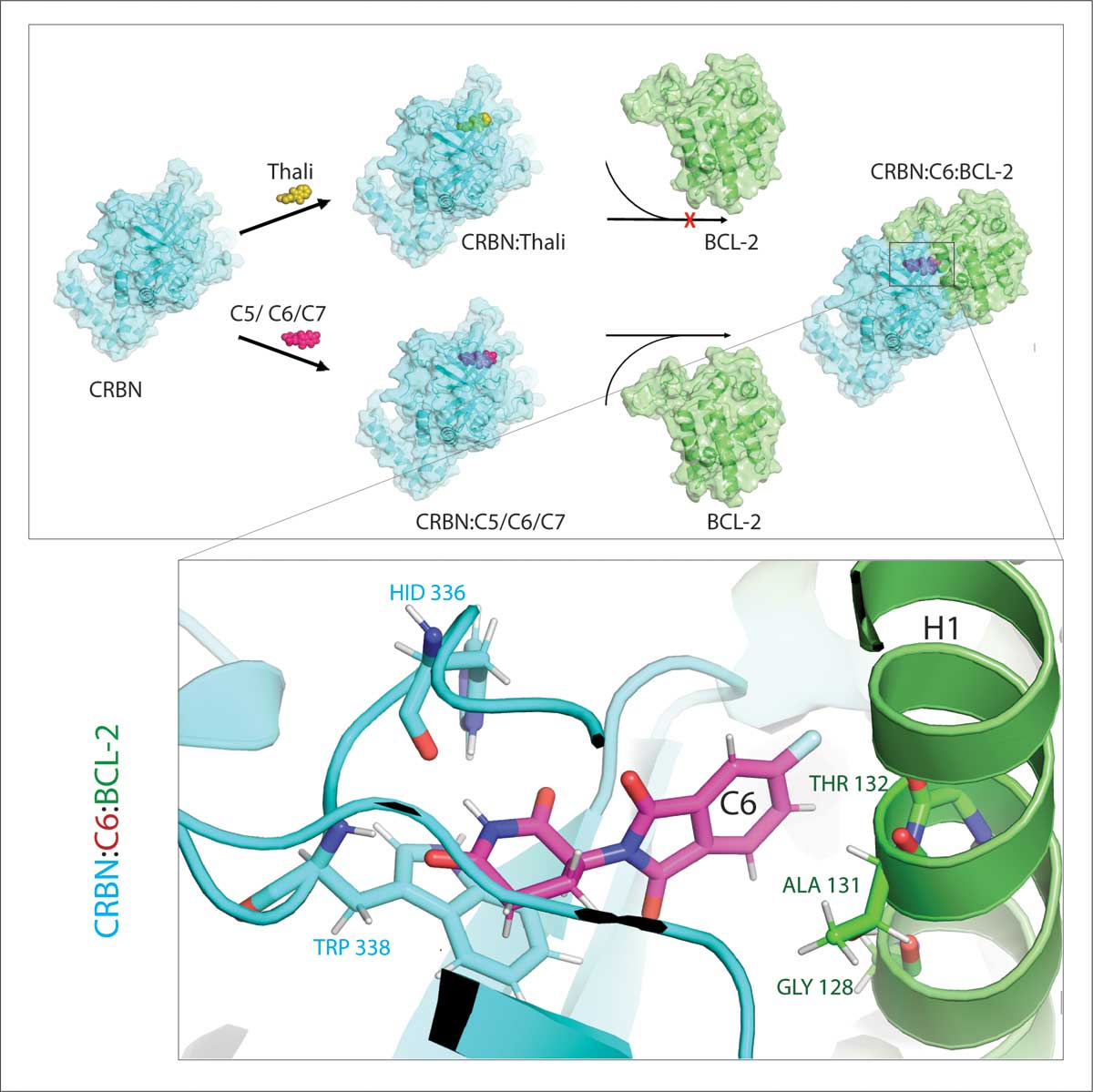
“We know now that thalidomide is something referred to as a ‘molecular glue’,” explains Dr. Xinlai Cheng from the Institute of Pharmaceutical Chemistry at Goethe University Frankfurt. “This means it is able to catch hold of two proteins and pull them together.” This is particularly interesting because one of these proteins is a kind of ‘labeling machine’: It attaches an unmistakable label to the other protein that says “WASTE”.
The cell’s waste disposal system recognizes this label: It catches hold of the marked protein molecule and shreds it. “It is precisely this mechanism that explains the different effects of thalidomide,” says Cheng. “Depending on which protein is marked, it can lead to malformations during embryonal development or else kill off malignant cells.”
This mechanism opens up great possibilities for medicine because cancer cells are dependent on certain proteins to survive. If these could be systematically targeted and shredded, it might be possible to cure the disease. The problem is that molecular glue is rather idiosyncratic. One of its binding partners is always the cell’s labeling machine, or in scientific terms an E3 ligase called CRBN. Only very few of the many thousands of proteins in the body come into question as the other partner – which ones exactly vary from glue to glue.
“That is why we produced a range of thalidomide derivatives,” says Cheng. “We then examined whether they have glue-like properties and, if so, which proteins they are effective against.” To do this, the researchers added their derivatives to all the proteins in a cultured cell line. They then monitored which of these proteins were subsequently degraded in the presence of CRBN.
“During the process, we pinpointed three derivatives that are able to mark a cell protein which is very important for degradation, BCL-2,” explains Cheng. “BCL-2 prevents the activation of the cellular self-destruction program, so if it is absent, the cells perish.” That is why BCL-2 has already been in the spotlight of cancer research for some time. There is even already a drug for treating leukemia, called venetoclax, which reduces the efficacy of BCL-2 and in this way causes mutated cells to self-destruct.
“In many cancer cells, however, BCL-2 itself is mutated. As a result, venetoclax no longer inhibits the protein,” says Cheng. “We were able to show that our derivatives also mark this mutated form for degradation. Moreover, our partners at the Max Planck Institute of Biophysics simulated the interaction of the thalidomide derivatives with BCL-2 on the computer. This showed that the derivatives bind to completely different sites than venetoclax – a result that we were later also able to corroborate experimentally.”
In addition, the researchers tested their substances in fruit flies with cancerous cells. The survival rate of flies treated in this way was much higher. However, Cheng warns against exceedingly high expectations, as these results are still basic research: “Although they show that modified thalidomide molecules have great therapeutic potential, we cannot say yet whether they will actually prove themselves in practice at some point in time.”
The work was supported by DFG, the Frankfurt Cancer Institute, and the PROXIDRUGS project.
Publication: Jianhui Wang, Marcel Heinz, Kang Han, Varun J. Shah, Sebastian Hasselbeck, Martin P. Schwalm, Rajeshwari Rathore, Gerhard Hummer, Jun Zhou, Ivan Dikic, Xinlai Cheng: Thalidomide derivatives degrade BCL-2 by reprogramming the binding surface of CRBN; Cell Reports Physical Science (2024) https://doi.org/10.1016/j.xcrp.2024.101960