Goethe University Frankfurt is applying for the upcoming round of the Excellence Strategy of the German federal and state governments with four new clusters on the following research topics: Trust in conflict (ConTrust), infection and inflammation (EMTHERA), the origin of heavy chemical elements (ELEMENTS), and cellular architectures (SCALE). These applications bring together the competencies and pioneering ideas of Goethe University Frankfurt with those of colleagues in the Rhine-Main Universities (RMU) alliance and additional partners from four major non-university research organizations. The Cluster of Excellence “Cardio-Pulmonary Institute” (CPI), first set up in 2019, will submit a full proposal next year.
The interdisciplinary Cluster of Excellence initiative EMTHERA (Emerging Therapeutics) aims to explore the molecular mechanisms that underlie diseases at the interface between infections, inflammation and impaired immunity. Two researchers from Goethe University Frankfurt are part of the project and contributing their expertise: Maike Windbergs, Professor of Pharmaceutical Technology, and Peter Wild, Professor of Pathology. Both have already accomplished a lot in their respective fields.
Artificial intelligence (AI) gives a second opinion
At the start of his lectures, Peter Wild – head of the Dr. Senckenberg Institute of Pathology (SIP) at University Hospital Frankfurt – likes to emphasize that he is not a forensic investigator the likes of whom appear in popular series like CSI or NCIS, but a pathologist. The two professions are not to be confused. Pathology is the study of diseases, a cross-sectional field of medicine that centers on tissue analysis. Intravital diagnostics, i.e. the analysis and evaluation of tissue samples from living beings, be they humans or animals, accounts for 95 percent of a pathologist’s worktime. The field has changed a lot over the last years, Wild says, adding that, for one, “digitalization allows us to collect vast amounts of data. One single histological image alone can be up to ten gigabytes in size.” Another development is new technologies such as next generation sequencing (NGS), which makes it possible to examine cells at the molecular level. These data are collected, too. Storing the growing mass of data requires technical solutions, which to Wild constitutes an opportunity to advance medical research.
His goal is to further develop pathology into a quantitative, computerized discipline that is precise, predictive, prognostic and personalized. Wild is working to put this 4P pathology into practice step by step. SIP researchers are in the process of building up an enormous biobank with histological images and molecular data of cancerous tissue, which to date contains some 40,000 patient datasets. An important step towards personalized medicine, says Wild: “Although each tumor looks completely different under the microscope, there are also similarities, which we are trying to classify with the help of the biobank. In this way, we want to categorize cancer patients in specific groups so that customized therapies can be derived.”
The scientists at SIP are also making use of artificial intelligence (AI), to help pathologists evaluate prostate carcinomas, for example. In this particular case, for instance, they are studying to what extent cancerous tissue differs from healthy tissue. This “difference” reveals how aggressive a prostate carcinoma is, i.e. how fast it is growing – and is determined by pathologists as part of what is known as a Gleason score. “The problem is that pathologists can grade the same tumor differently,” says Wild. The first pathologist identifies a 3+3 carcinoma, meaning there is no need to operate in the case of smaller tumors. The second grades it as a 3+4 carcinoma, making surgery unavoidable. This phenomenon, called interobserver variability, leads to certain aberrations: carcinomas are classified as either too dangerous or too harmless – resulting in wrong therapeutic decisions.
How can AI ensure that this no longer happens? First, it is trained with data from a large number of carcinomas and pathologists’ respective evaluations, to which it then gives its own “second opinion” on a specific carcinoma. The pathologist examines this opinion and checks it against his or her own evaluation again, insofar as the AI came to a different conclusion. “What we are in effect using here is the ‘wisdom of the crowd’,” explains Wild. “Although, with the models commonly used today, AI will never be as good as the best pathologist, it will always be as good as the average pathologist. Its evaluations are therefore based on a solid foundation.” This also applies to breast cancer diagnostics, where the Ki67 value, which indicates what percentage of tumor cells are in the growth phase, plays an important role. The figure is decisive to determine whether the patient needs chemotherapy or not. Here, too, there can be aberrations in the “human” assessments, which the machine’s second opinion is intended to prevent.
Another important development step consists of making the raw data from pathological examinations available to the research community as part of Open Science. This is where a new project – the Goethe University Data Repository (GUDe) – comes into play, within which research data can be stored, shared and published for a period of at least ten years. The SIP recently started to collect and store twice pseudonymized, i.e. non-traceable, clinical carcinoma image data in a structured manner. In the future, researchers from around the world will be able to view and use these datasets. Wild contextualizes the importance of Open Science: “You can advance medical research by developing a new drug or inventing an ingenious tool. But you just as well move it massively forward by making structured datasets available.” One case in point is new drug development. “Many clinical trials fail because of the high costs associated with amassing the required prior knowledge. If this were available in a well-structured manner, costs would drop. Open Science enables us to develop drugs that may not have seen the light of day without its existence.”
No more animal testing?
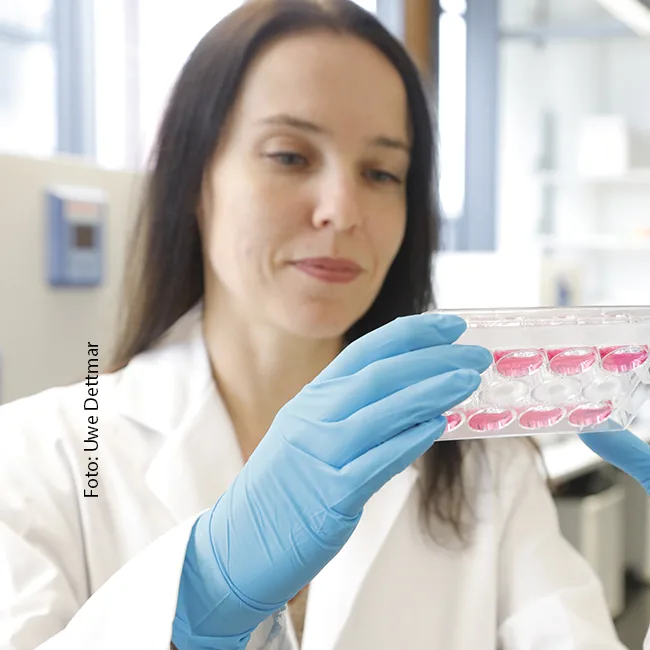
Evaluating the effect of a new drug in humans means testing it beforehand. One way is animal experimentation, usually with mice. However, this often results in intense pain for the animal or even death. Apart from ethical issues, there is also the question of predictivity: How precisely can we evaluate the effect of a drug in humans if it is only tested on animals? After all, animals have a different body frame than humans, and the physiological processes taking place in an animal’s body also differ from those of human bodies. That is why it is impossible to simply transfer the results 1:1 to humans. “It’s better to use human tissue for drug tests from the very get-go,” says Maike Windbergs from the Institute of Pharmaceutical Technology. She is working in precisely this field of research, also known as the “3Rs”, whereby the 3Rs stand for the replacement, reduction and refinement of animal experimentation.
Windbergs studied pharmacy in Düsseldorf and completed her doctoral degree on the subject of drug delivery, i.e. how a drug must be packaged for it to reach its target in the body and take effect there. She then went on to become a postdoctoral researcher at Harvard’s John A. Paulson School of Engineering and Applied Sciences, where she worked with microfluidic reactors, used to cultivate human or animal tissue in a flowing fluid, just like blood, lymphatic fluid and saliva flow in the human body. Windbergs explains: “This movement is ignored in a normal cell culture vessel, and although the cell culture medium is a liquid, it is nevertheless static.” After Harvard, she joined the Helmholtz Institute for Pharmaceutical Research Saarland (HIPS) in Saarbrücken in 2010, where she intensified her work on the 3Rs principle and grew organ systems based on human cells and tissues. Then, in 2017, Windbergs accepted the call to a new professorship for 3Rs alternatives at Goethe University Frankfurt, where she is currently working on methods to make animal experiments superfluous.
The human tissue for her experiments comes from beauty clinics, among others, which collect the waste tissue from plastic surgery and deliver it to her laboratory at the university for further processing. Windbergs’ focus is on developing in-vitro models based on human tissue to imitate wound healing. In fact, wounds illustrate very clearly why it is better to use human tissue to test drugs for humans. “Let’s take the mouse, for example. Since it is a wild animal, its wounds must close over very quickly so that it doesn’t die.” That is why the mouse – like other rodents – has an additional subcutaneous muscle, the panniculus carnosus, which pulls the tissue together over the wound. “We humans don’t have this muscle; our wounds heal solely via cells that enter the wound bed and close the wound in the process. Although something similar also occurs in mice, the dominant mechanism is the contraction of the additional muscle. The way a mouse heals its wounds is therefore different to ours.”
Healing wounds is one matter, but for hospitals, treating infected ones is an enormous problem. Bacteria form biofilms that make it extremely difficult to control the infection. “We recently achieved a real breakthrough,” says Windbergs. Scientists have dedicated many years of research to developing an in-vitro model of a wound with a bacterial biofilm. The problem is that a cultivated biofilm matures only very slowly. So slowly, in fact, that the cells beneath it die off once the maturation process is completed. That is why Windbergs has developed another method for infected wounds: The biofilm matures separately and is then applied intact to the tissue model. She is pleased with the results: “The model is very predictive and provides useful information about the processes taking place in the human body. Theoretically speaking, industry could start testing new active substances tomorrow.” In the next step, Windbergs is working on further variations of the tissue-biofilm combination and testing biofilms that contain several dangerous bacterial germs: the six most virulent pathogens worldwide, summarized under the acronym ESKAPE. Another project focuses on cultivating a three-dimensional small intestine model made out of human tissue, with the gut-brain axis at its center, i.e. the communication network in which the intestine and the brain influence each other. There is increasing evidence that the permeability of the intestine can promote neurodegenerative diseases such as Alzheimer’s.
Andreas Lorenz-Meyer
EMTHERA
Open Science plays a key role in the EMTHERA project, Peter Wild says. The data produced by the researchers participating in the initiative are categorized and made publicly accessible, in the hopes that they will enable scientists to develop models for infectious, inflammatory and immunological diseases. 3Rs models will also be an essential part of EMTHERA, adds Maike Windbergs. Drug delivery systems are another special field within the initiative: Both the working group led by Windbergs as well as researchers in Mainz are working in this area, which centers on the packaging of molecules such as mRNAs and PROTACs.
More information here.