New strategies for targeted drug delivery
Even the best drug in the world is completely useless if the active substance fails to reach the site of action in the body where it is supposed to fight the disease. Pharmacist Maike Windbergs is an expert in drug carrier systems, whose aim is to ensure targeted delivery. For her research, she also uses human brain, intestinal or skin tissue cultivated in the laboratory.

The wound dressing is light-colored and as soft as a baby wipe. That it is, in fact, an extremely complex high-tech fabric is invisible to the naked eye, and its fibers are made of something really special.
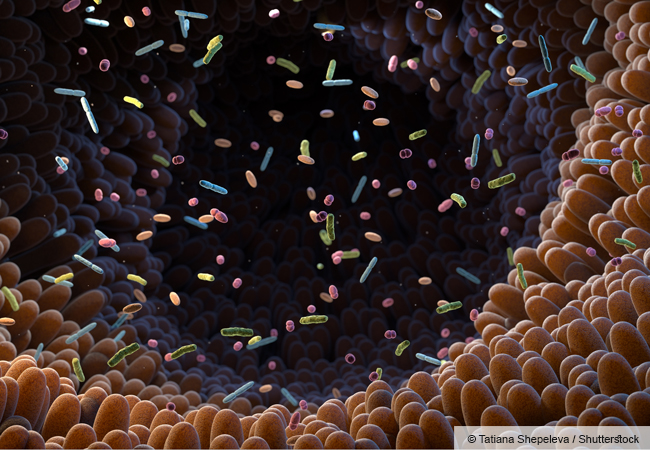
Although they are just one-fiftieth the thickness of a human hair, the fibers constitute a sophisticated core-shell structure. Their outer layer consists of a synthetic polymer called polyvinylpyrrolidone (PVP). More interesting, however, is the core encapsulated in the PVP. It contains viruses – and quite useful ones at that: bacteriophages. These do not infect human cells but instead attack bacteria. This content makes the fabric a beacon of hope for the treatment of chronic wounds.
The Institute of Pharmaceutical Technology at Goethe University Frankfurt houses the loom used to produce the fabric. It is headed by Professor Maike Windbergs, 44, an expert in delivering active substances against diseases to the place in the body where they are needed. “We used a process called electrospinning to produce our wound dressings,” she says.
High voltage draws polymers apart to form fine fibers
In this process, a very high voltage (several thousand volts) is applied to a nozzle and a rotating spindle. The polymer solution exiting the nozzle is attracted by the oppositely charged spindle, which causes the fine jet of liquid to expand. The solvent evaporates at the same time, producing ultrafine fibers that are caught by the rotating spindle. “Our special spinneret enables us to embed the bacteriophages in the fibers during this process,” explains Windbergs.
When the fabric produced in this way is placed on a wound, the bacteriophages are gradually released. This takes place over hours or even days so that the bacteria preventing the wound from healing are subjected to an ongoing attack over a longer period. “Even resistant species are no match for this,” says Windbergs. “The high-tech dressings thus represent a promising approach for bringing wounds under control that can hardly be treated clinically.”
Maike Windbergs has been working on drug carriers since completing her doctoral degree at Heinrich Heine University Düsseldorf. Drug carriers play an important role in the development of treatment strategies against dangerous diseases: They should not only ensure that drugs reach the site of action in the body but also that these are as effective as possible once they arrive there. In pharmacy, this is also called “targeting”.
Targeting is a collective term for various methods that sometimes go hand in hand. “We differentiate between passive and active targeting,” says Windbergs. “Passive targeting means that we make use of certain properties of the diseased tissue to enrich the active substance.” Wound infections are a good example to illustrate this: The bacteria responsible for such an infection create an environment in which they can thrive particularly well, for example by lowering the pH value in the wound. In addition, certain enzymes, called metalloproteases, are released. These cleave proteins in the infected tissue, which worsens the inflammation.
Different conditions prevail in wounds than in healthy skin
“This means that we have a different microenvironment in a wound than we do in healthy skin,” explains Windbergs. “And we can make targeted use of this phenomenon – for example by packaging active substances in a carrier that dissolves particularly quickly at a low pH value or which metalloproteases can easily cleave.” The pathological changes in the tissue ensure that the active substance is released exactly where it is needed.
Active targeting even goes one step further: It directs the drug systematically to certain cells or even individual molecules that play an important role in the disease. A molecular “address label” is attached to the carrier, as it were. “This is often an antibody that binds to specific target structures,” explains Maike Windbergs. The two strategies can also be combined.
Today, targeting is a very important aspect in the development of new therapeutics because it is possible to achieve a greater effect with a smaller amount of active substance. On the one hand, this makes treatment more cost-effective. In addition, the risk of unwanted side effects is considerably reduced thanks to better targeting accuracy.
Customized strategy for each disease

All drugs require their own customized approach. “Take the RNA vaccines developed by BioNTech or Moderna against SARS-CoV-2, for example,” says Windbergs: “They were packaged in lipid nanoparticles, in lay terms small fatty spheres.” RNA is negatively charged; positively charged lipids can be used to encapsulate the RNA molecules. “The charge also activates the immune system, which is what a vaccine aims to achieve.”
Vaccines protect us against infections, but RNA molecules can also be used to cure us of existing diseases. In this case, a strong immune response is not necessarily conducive. “To prevent this, we have to find a completely different type of packaging,” says Windbergs.
Drug targeting thus calls for strategies that are not available “off the shelf”, which is why scientists also need suitable test systems to check whether their carriers are fit for the purpose. To do this, the Windbergs Group at the Institute of Pharmaceutical Technology uses human tissue removed during surgery, provided that the patients have given their previous consent. But many are willing to donate. “We test our wound dressings on skin flaps from operations, for example,” explains Professor Windbergs.
Complex tissue “reproduced” in the laboratory
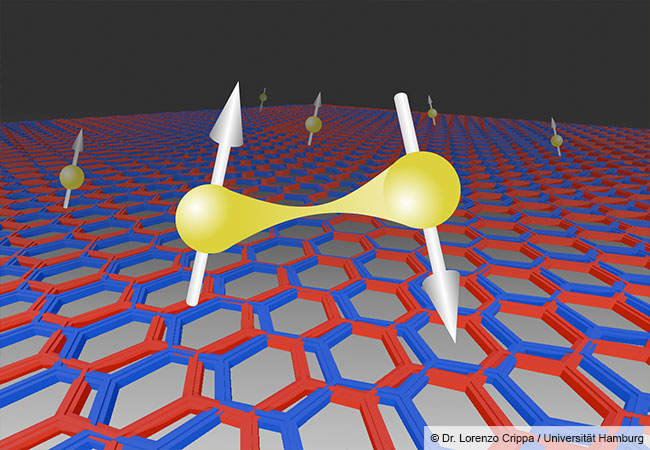
However, the scientists also use human cells to produce tissue themselves. One example is the blood-brain barrier, which prevents harmful molecules, bacteria or viruses from entering the brain from the bloodstream via the blood vessel walls. To this end, the blood vessels that supply our brain with oxygen and energy are lined with special endothelial cells, which seal the blood vessels and allow only certain substances to pass through. To do this, they work hand in hand with other types of cells – on the brain side, for example, with the microglia cells, a special type of phagocyte (scavenger cell). Microglia cells can absorb and digest foreign substances and are thus part of the immune system.
Several other protagonists also play a role in the blood-brain barrier. “Despite its complex structure, it is meanwhile possible to cultivate the blood-brain barrier in the laboratory from different cell types,” explains Windbergs. “And not just the blood-brain barrier of healthy people but also of people with neurodegenerative diseases such as Alzheimer’s.” It is now known that this important barrier is damaged in people suffering from such diseases and becomes more permeable. Presumably responsible for this are fragments of amyloid plaques, characteristic deposits of proteins and fat-like molecules found in large numbers in the brains of people with Alzheimer’s disease.
The Windbergs Group uses the artificial tissue to explore various research questions. “For example, we reproduce an intact blood-brain barrier in a test tube and then examine what toxic effect certain plaque components have on it,” she explains. This model system is also a helpful tool in the search for strategies to deliver potential active substances to damaged areas of the brain despite the barrier.
Creating body-like conditions

Growing intestinal mucosa, brain tissue or parts of other organs in the laboratory is a complex undertaking. Depending on the type of tissue, different experimental protocols apply and must be followed. Individual components often need to be pre-cultivated separately, each in a special culture medium and under specific conditions. Strict rules apply when mixing them, too: Which type of cell is added when? And in what amount?
Ideally, the various components then arrange themselves automatically – just as they would in the human body. “For this to work, however, cultivation conditions must be exactly right and as similar as possible to those in the organism,” says Windbergs. When cultivating a mucous membrane of the small intestine, for example, the culture medium must be agitated so that the folds typical of this type of tissue are able to form. After all, the digested food that flows through the intestine is also on the move. “The cells need a certain degree of mechanical shear stress,” continues Windbergs. “But the amount is very important: If the culture is subjected to excessive mechanical stress, the cells die.”
The cultivation of human tissue thus calls for a precisely orchestrated procedure. In many cases, the individual steps required for this have been optimized by researchers around the world in many years of work. The effort is nevertheless worthwhile: Scientists can use the organs produced in this way to answer questions for which experiments with animals, for example, would not be particularly promising. After all, a lab mouse is a mouse. Cultivated tissue is something else: It consists entirely of human cells.

About / Maike Windbergs, born in 1980, has been a professor at Goethe University Frankfurt since 2017, where she heads the Institute of Pharmaceutical Technology. Windbergs studied pharmacy in Düsseldorf and completed her doctoral degree in pharmaceutical technology there and at the universities of Helsinki (Finland) and Enschede (Netherlands). After a research stay at Harvard University in the USA, she was a junior research group leader at the Helmholtz Institute for Pharmaceutical Research Saarland (HIPS) and at Saarland University, where she completed her Habilitation before joining Goethe University Frankfurt. She has received several prestigious scientific awards for her research achievements.
windbergs@em.uni-frankfurt.de

The author / Frank Luerweg, born in 1969, graduated in biology. He was deputy press spokesperson at the University of Bonn and has been working as a freelance science journalist for 13 years.