Acute lymphoblastic leukaemia (ALL) is the most common kind of cancer in children. T-ALL, a subtype that resembles T-lymphocytes, can be treated successfully with the drug nelarabine. The drug has not been successful, however, with B-ALL, a subtype resembling B-lymphocytes. Since the 1980s, oncologists have been puzzled as to the cause of this difference. Now, an international research team headed by Goethe University and the University of Kent has discovered the reason: B-ALL cells contain the enzyme SAMHD1, which deactivates the drug.
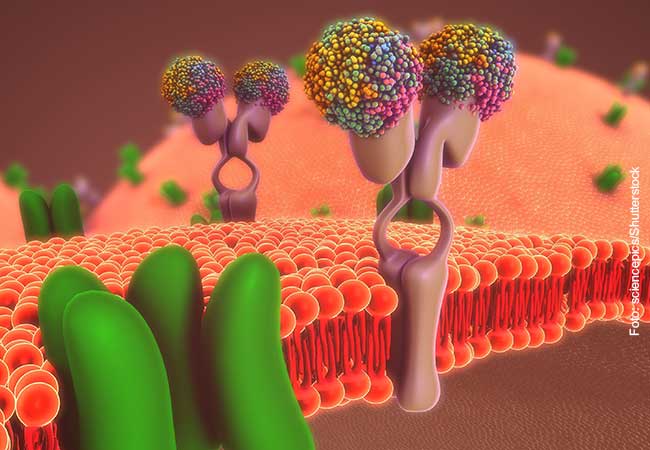
In the current issue of “Communications Biology”, Professor Jindrich Cinatl from the Institute for Medical Virology at Goethe University and Professor Martin Michaelis from the School of Biosciences at the University of Kent report on their investigations with nelarabine on different cell lines. “Nelarabine is the precursor of the drug, a prodrug, that does not become effective until it is combined with three phosphate groups in the leukaemia cell,” explains Professor Cinatl. “In studies of various ALL cell lines and leukaemia cells from ALL patients, we have been able to demonstrate that the enzyme SAMHD1 splits the phosphate groups off so that the medicine loses its effect.” Because B-ALL cells contain more SAMHD1 than T-ALL cells, nelarabine is less effective with B-ALL.
These results could improve the treatment of ALL in the future. In rare cases, B-ALL cells contain very little SAMHD1 so that treatment with nelarabine would be possible. On the contrary, there are also rare cases of T-ALL exhibiting a lot of SAMHD1. In such cases, the otherwise effective nelarabine would not be the right medication. Professor Michaelis observes: “SAMHD1 is thus a biomarker that allows us to better adapt treatment with nelarabine to the individual situation of ALL patients.”
Tamara Rothenburger, whose doctoral dissertation was funded by the association “Hilfe für krebskranke Kinder Frankfurt e.V“, is satisfied when she looks back at her research. “I hope that many children with leukaemia will benefit from the results.” The research was also supported by the Frankfurt Stiftung für krebskranke Kinder. Additional members of the research group are Ludwig-Maximilians-Universität Munich, and University College London.
Publication: Tamara Rothenburger, Katie-May McLaughlin, Tobias Herold, Constanze Schneider, Thomas Oellerich, Florian Rothweiler, Andrew Feber, Tim R. Fenton, Mark N. Wass, Oliver T. Keppler, Martin Michaelis, Jindrich Cinatl. SAMHD1 is a key regulator of the lineage-specific response of acute lymphoblastic leukaemias to nelarabine, in: Communications Biology, DOI 10.1038/s42003-020-1052-8, https://www.nature.com/commsbio/